Candida Auris
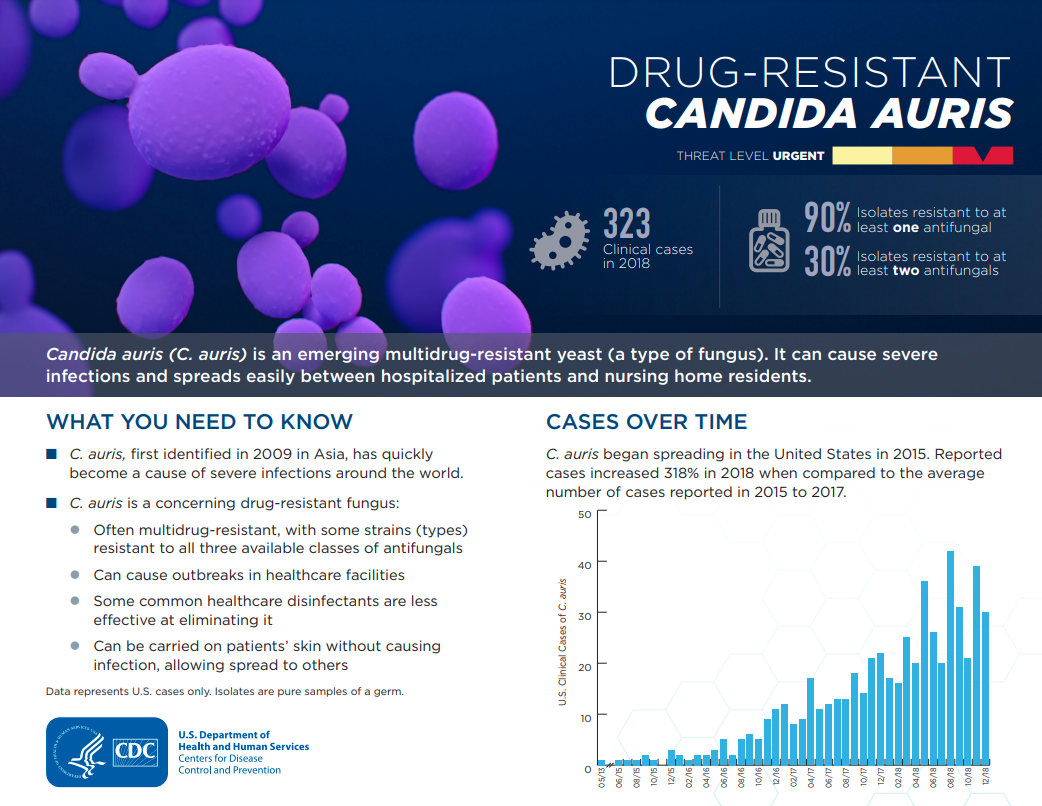
Candida Auris is a species of ascomycetous fungus, of the Candida genus, which grows yeast. It was first reported in the United States by the Centers for Disease Control and Prevention (CDC) in 2013. C. auris is commonly referred to as a healthcare acquired infection (HAI) because it is most often found in patients in long term or intensive care settings in healthcare facilities. Candida Auris is also known to be resistant to known treatments.
What are the types of candida cases?
C. auris cases are divided into two main categories, clinical cases and colonized cases.
-
Clinical cases are cases of C. auris that are identified from a specimen collected during clinical care for the purpose of diagnosing or treating diseases, such as a wound, urine, sputum, or blood.
-
Colonized cases of C. auris are identified upon swabbing a person’s axilla (under arm) and groin regions to test for colonization (when a person is carrying the organism somewhere on their bodies without symptoms of active infection. Colonized cases can also be referred to as screening cases.
What are the symptoms?
C. auris can cause several types of infection such as blood, wound, or ear infections. Sometimes symptoms are not noticeable because patients with C. auris are often receiving care for another serious condition or illness and are in a hospital or long-term care unit. A laboratory test needs to be conducted to determine whether a patient has C. auris. Patients who are colonized (C. auris living on the body) with this fungus are often asymptomatic and do not show additional signs of infection. Roughly 5-10% of individuals who are colonized with C. auris develop some type of infection within one year.
How is it spread?
C. auris is transmitted person to person through direct contact with infected bodily tissues or fluid. It can cause infections when it enters the body. Often it enters through medical devices such as ventilators, intravenous catheters, or wounds from surgery. C. auris can live on surfaces for at least 14 days. In healthcare facilities C. auris has been spread through contact with highly touched surfaces within a patient’s room or through shared medical equipment.
How can it be prevented?
Prompt identification and implementation of recommended infection control measures is the best way to prevent additional patients from being infected or colonized. Healthcare settings can help prevent the spread of C. auris by cleaning medical equipment properly, following all PPE (Personal Protective Equipment) and hand washing procedures, as well as proper surgical sterilization procedures and antibiotic stewardship practices. Additionally, patients who test positive in a healthcare setting should be placed under contact precautions. In facilities with cases of C. auris, screening tests when admitting new patients is recommended.
Where is it being reported?
Recently the CDC issued a statement about the concern for the growing numbers of cases in the United States. Candida auris cases have risen from 1 infection to more than 400 cases reported in Ohio since May of 2020. For more information about cases in Ohio please visit the Ohio Department of Health (ODH) website: odh.ohio.gov/know-our-programs/antibiotic-resistance/antimicrobial-threats/candida_auris
What does Cincinnati Health Department do when a case is reported?
Each case diagnosed in Cincinnati’s jurisdiction is investigated by our Communicable Disease Prevention and Control Unit according to ODH Infectious Disease Control Manual guidelines. You can find the guidelines here: odh.ohio.gov/know-our-programs/infectious-disease-control-manual/section3/section-3-candida-auris
Additional Resources from the CDC
-
General information about Candida Auris: cdc.gov/fungal/candida-auris/index.html
-
Resources for patients and family members: cdc.gov/fungal/candida-auris/patients-qa.html
-
Resources for health professionals: cdc.gov/fungal/candida-auris/health-professionals.html
-
Candida Auris surveillance: cdc.gov/fungal/candida-auris/tracking-c-auris.html
Latest News
-

- Jun. 13
- Bats and Rabies





